
- This event has passed.
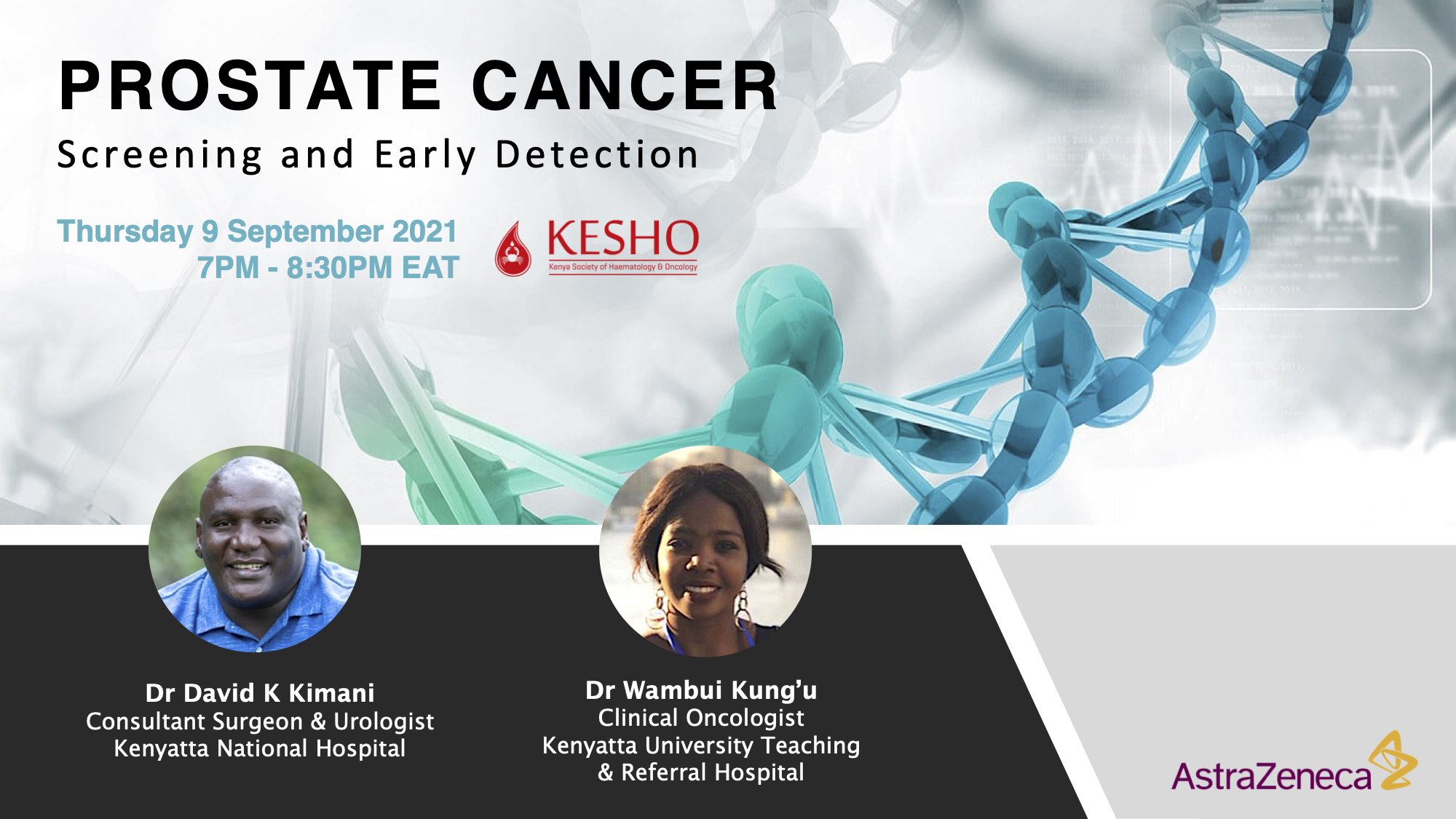
Prostate Cancer
Event Navigation
SPEAKER PROFILES:
1. Dr. David K Kimani
MBChB, MMed General Surgery UON (2007)
Dr. Kimani is a Consultant Urologist at Kenyatta National Hospital in Kenya, and Honorary Lecturer Department of Surgery at the University of Nairobi. He did his Clinical Fellowship in Urology at the Global Health Institute Chennai, India in 2014. He has keen interests in Prostate Care and Kidney Transplantation.
Dr. Kimani is a Member of SSK, KAUS, and the Society for International Urologists, (SIU), and the American Urological Association (AUA).
2. Dr. Wambui Kung’u
Dr. Wambui Kung’u is a Clinical Oncologist at Kenyatta University, Teaching, Referral, and Research Hospital. She holds a Master’s Degree in Clinical Oncology and Nuclear Medicine from Alexandria University, Egypt.
She is a member of the Kenya Society of Hematology and Oncology (KESHO), African Organization for Research and Training in Cancer (AORTIC), European Society of Medical Oncology (ESMO), and American Society of Clinical Oncology (ASCO).
Her main areas of interest are Head and Neck cancers, breast cancer, prostate cancer, and gastrointestinal cancer.

