
- This event has passed.
Endometrial Cancer
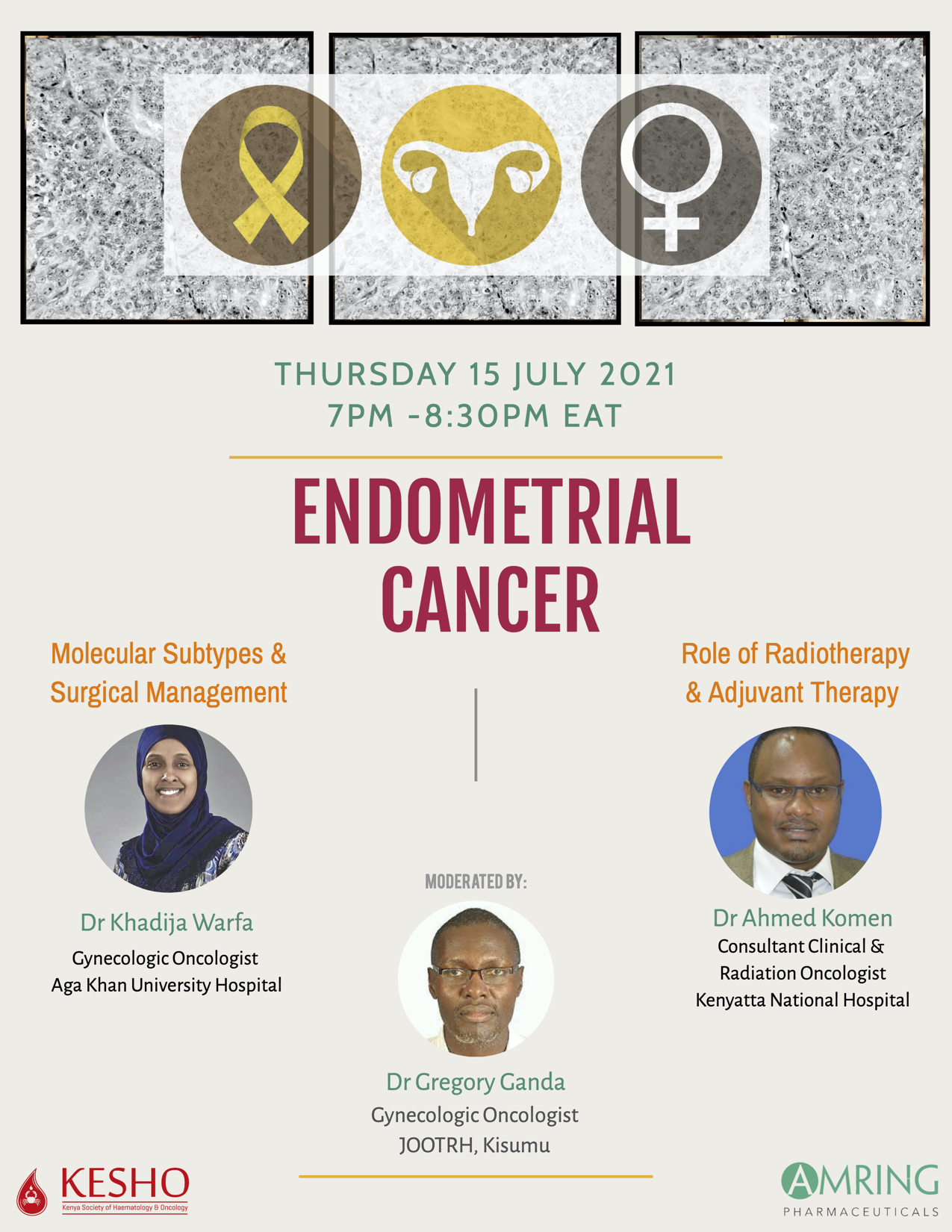
Moderator: Dr. Gregory Ganda, Gynaecology oncologist Jaramogi Oginga Odinga Teaching and Referral Hospital (JOOTRH Sponsor: AMRING Presenters:
- Dr. Khadija Warfa, Gynecologic oncologist, Aga Khan University Hospital
- Dr. Ahmed Komen, Clinical and Radiation Oncologist, Kenyatta National Hospital/AKUH.
To date, many cancers are affecting the uterus. Endometrial cancers (EC) affect the endometrial lining of the uterus and are more common in North America and parts of Russia and China. They are less common in sub-Saharan Africa, and mostly affect postmenopausal women with an average age of 64 years. Obesity is a major risk factor for EC oncogenesis. Hereditary risk factors for EC pathogenesis include Lynch and Cowden syndromes. Proper diet and regular exercise, use of hormonal contraception, multiple childbirths, and breastfeeding decrease the risk of EC. Clinical presentation of EC is mainly abnormal/postmenopausal bleeding, while advanced disease presents with pelvic and abdominal symptoms resembling ovarian cancer. Diagnosis is by office pipelle biopsy and hysteroscopy biopsy. Women with ET >4-5mm on transvaginal ultrasound and also post-menopausal women with endometrial fluid >11mm and are asymptomatic should get a biopsy. The gold standard for imaging is MRI. The primary treatment for uterine-confined endometrial carcinoma is TH/BSO and lymph node assessment, where sentinel node assessment has been shown to reduce complications related to complete lymphadenectomy. Molecular classification of EC is encouraged in all endometrial carcinomas, especially in high-grade tumors. In molecular dualistic classification, type I tumors are estrogen-dependent, and associated with endometrial hyperplasia, while Type II tumors are estrogen-independent and associated with endometrial atrophy with a poorer prognosis. The WHO histologic classification involves endometrial epithelial tumors and serous endometrial cancer. Clear cell carcinoma accounts for <10% of endometrial adenocarcinoma. They demonstrate molecular heterogeneity and can overlap with serous and endometrial carcinoma. Carcinosarcoma represents 5% of EC. The benefit of molecular classification is that the method is based on more objective variables and it identifies significantly more patients with favorable features that would otherwise be classified as a high intermediate risk with pathology review alone. Unlike other cancers, FIGO staging does not determine the patient outcome, because some of the prognostic characteristics of the disease have not been incorporated in the staging. Early presentation following post-menopausal bleeding results in a generally good prognosis but should be treated using an evidence-based protocol. Considerations for adjuvant treatment include the extent of surgery, adequacy of the pathology report, risk stratification, and molecular classification. Lymphadenectomy should be considered for high intermediate-risk patients for adequate staging and optimal tailoring of adjuvant treatment. Radiotherapy can be used for definitive treatment on patients not candidates for surgery, patients with recurrent disease, and also for palliation. In a rural setup where resources are constrained, an ultrasound can be done, followed by a referral to a facility with the necessary resources and personnel.